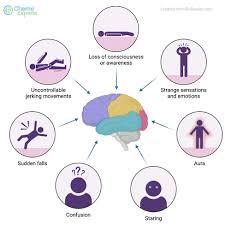
Seizures
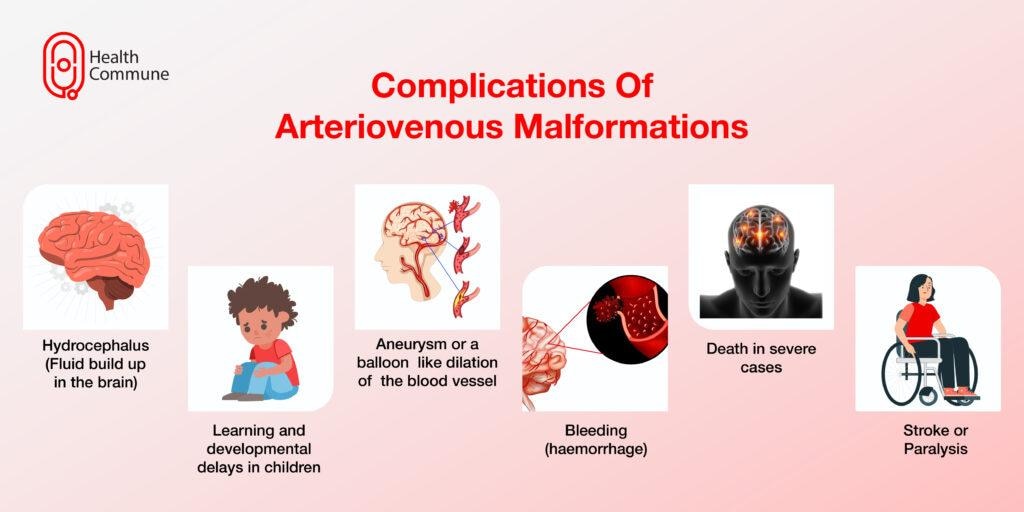
Seizures:-What is a seizure?A seizure (pronounced “see-zhr”) is a surge of abnormal electrical activity in your brain. The most recognizable symptoms of a seizure are a temporary loss of consciousness and uncontrollable movements (convulsions).Not all seizures look the same. You might stop what you’re doing and stare off into space for a few seconds. You might jerk your arm or feel your muscles twitch. You might only have one seizure in your life or have multiple seizures per day. Your experience with seizures can be very different from someone else’s.There are many possible causes of seizures because a lot of things can interfere with your brain’s typical electrical patterns. These range from changes to your blood sugar levels to an illness, injury or underlying condition.SymptomsSymptoms vary based on the type of seizure. They also can range from mild to serious. Seizure symptoms may include:Short-lived confusion.A staring spell.Jerking movements of the arms and legs that can't be stopped.Loss of consciousness or awareness.Changes in thinking or emotions. These may include fear, anxiety or a feeling of already having lived the moment, called deja vu.Most seizures fall into one of two classes called focal or generalized. The classes are based on how and where the brain activity causing the seizure began. If health professionals don't know how the seizures began, they may say the seizures are of unknown onset.What are the types of seizures?There are two main types of seizures:Generalized seizures (generalized onset seizures): Electrical activity starts on both sides of your brain at the same time. You may shake both sides of your body, shake one side or only stare and stop what you’re doing. Usually, it affects kids or young adults, but it can occur at any age.Focal seizures (focal onset seizures): Electrical activity begins on one side or “focus” of your brain. Symptoms usually affect one side of your body and may or may not affect your awareness. This means that you may or may not remember the seizure. Focal seizures may stay focal or may spread to both sides.Generalized seizure typesThe types of generalized seizure disorders include:Absence seizures: You stop what you’re doing and have a blank stare.Atonic seizures (drop seizures): You lose muscle control and drop to the ground suddenly.Clonic seizures: You’ll shake both sides of your body and pass out or shake one side and not pass out.Myoclonic seizures: These involve a quick jerk or twitch that affects one muscle or a group of connected muscles.Secondary generalized seizures: You have a focal seizure (electrical activity starts in one part of your brain) followed by a generalized seizure (electrical activity spreads to both sides of your brain).Tonic-clonic seizures: Your muscles stiffen, you lose consciousness and have convulsions.Tonic seizures: You pass out and your muscles tighten up but you don’t have convulsions.Focal seizuresFocal seizures result from electrical activity in one area of the brain. This type of seizure can happen with or without passing out, called losing consciousness.Focal seizures with impaired awareness. These seizures involve a change or loss of consciousness or awareness that feels like being in a dream. During these types of seizures, people may seem awake. But they stare into space and don't respond to anything around them.They may repeat movements such as hand rubbing and mouth movements, repeat certain words, or walk in circles. They may not remember the seizure or even know that it happened.Focal seizures without impaired awareness. These seizures may change emotions. They also may change how things look, smell, feel, taste or sound. But people having a focal seizure don't pass out.During these types of seizures, people may feel angry, joyful or sad. Some people have nausea or odd feelings that are hard to describe. These seizures may cause trouble speaking and jerking of a body part such as an arm or a leg. They also may cause sudden symptoms such as tingling, dizziness and seeing flashing lights.Symptoms of focal seizures may seem like those of other conditions of the brain or nervous system. These other conditions include migraine, mental illness or a condition that affects how the brain manages sleep-wake cycles, called narcolepsy.Generalized seizuresSeizures that appear to involve all areas of the brain from the time they start are called generalized seizures. Types of generalized seizures include:Absence seizures. Absence seizures often happen in children. These seizures once were called petit mal seizures. People who have absence seizures most often stare into space or make slight body movements such as eye blinking or lip smacking. The seizures most often last for 5 to 10 seconds.Absence seizures can happen up to hundreds of times a day. They can come in clusters. And they can cause a brief loss of awareness.Tonic seizures. Tonic seizures cause muscles to get stiff. These seizures most often affect muscles in the back, arms and legs. People who have these seizures may pass out and fall to the ground.Atonic seizures. Atonic seizures cause a sudden loss of muscle use, most often in the legs. They're also called drop seizures. People having this type of seizure may collapse.Clonic seizures. Clonic seizures are linked with jerking muscle movements. These seizures usually affect the neck, face and arms on both sides of the body.Myoclonic seizures. Myoclonic seizures most often cause sudden brief jerks or twitches of the arms and legs. People who have these seizures don't often pass out.Tonic-clonic seizures. Tonic-clonic seizures are the most common type of generalized seizure. They once were called grand mal seizures. They can cause passing out, body stiffness and shaking. They sometimes cause people to urinate or to bite their tongues.Tonic-clonic seizures last for several minutes. Tonic-clonic seizures may start as focal seizures that spread to involve most or all of the brain.Seizure stagesSeizures can have a beginning phase, a middle phase and an end phase. These phases also are called prodrome, ictal and postictal.Prodrome. This is the earliest warning that a seizure may happen. During the prodrome, people may have a hard-to-describe sense that a seizure may happen. They also may have changes in behavior. This can happen in the hours or even days before a seizure.The prodrome stage may include an aura. The aura is the first symptom of a seizure. Symptoms during the aura may include the feeling that a person or place is familiar, called deja vu, or a feeling that a person or place is not familiar.Or people may simply feel strange, feel fear or panic, or even have good feelings. Symptoms also may include smells, sounds, tastes, blurred vision or racing thoughts. Most often, auras are feelings that are hard to describe. The prodrome may include headache, numbness, tingling, nausea or dizziness.Many people with seizures have a prodrome or aura. But some people do not.Ictal phase. The ictal phase lasts from the first symptom, including the aura, to the end of the seizure. Symptoms of the ictal phase depend on the type of seizure.Postictal phase. This is the period after a seizure during recovery. The postictal stage can last minutes or hours. Some people recover quickly, while others take hours. The length of the postictal phase depends on the type of seizure and what part of the brain was affected.During this phase, people may be slow to respond, have trouble with memory, and have trouble talking or writing. They may feel sleepy, confused, dizzy, sad, scared, anxious or frustrated. They also may have nausea, a headache or weakness. They may feel thirsty or urinate.What are the symptoms of a seizure?Seizure symptoms vary based on the type and severity, but may include:Loss of consciousness.Uncontrollable movements (convulsions, muscle spasms, jerking).Staring.Other symptoms may include:Sudden emotional changes (confusion, fear, joy, anxiety).Teeth clenching.Drooling.Abnormal eye movements.Loss of bladder or bowel control.Noise making (grunting or snorting).These symptoms are temporary and only last for a few seconds to minutes.What are the warning signs of a seizure?Warning signs of a seizure may include:Sensory symptoms: Seeing bright lights or distortions in how objects appear, hearing unexpected sounds, sudden unexpected tastes (metallic or bitter) or smells and strange feelings on your skin (numbness or tingling).Emotional changes: Strong emotions like fear or joy, déjá vu (when a new experience somehow feels familiar) or jamais vu (when a familiar experience somehow feels new).Autonomic symptoms: These affect body systems that your brain runs automatically, like sweating, making too much saliva (drooling), an upset stomach and pale skin.Not everyone experiences warning signs before a seizure.What causes a seizure?A surge of electrical activity in your brain causes a seizure.Neurons (nerve cells) communicate by sending electrical signals to different parts of your brain. When a seizure happens, the affected brain cells fire signals uncontrollably to others around them. This kind of electrical activity overloads the affected areas of your brain and causes seizure symptoms.Seizure causes fall into two main categories depending on why they happen:Provoked seizures (nonepileptic): A trigger, which could be a temporary condition or certain circumstances, causes seizure symptoms to happen.Unprovoked seizures (epileptic): Seizures happen spontaneously (randomly). They may happen often. These seizures are the primary symptom of epilepsy.Seizures without a known cause are called idiopathic seizures.Seizure triggersThe following may trigger a seizure:Abnormal blood sugar levels (low or very high blood sugar).Certain medications, such as Wellbutrin® or bupropion.Flashing or flickering lights.Heat illness.High fever.Sleep deprivation.Stress.Substance use (including alcohol withdrawal).Triggers are different for each person. If you have seizures regularly, you may want to keep track of what you were doing before a seizure took place. A healthcare provider can review this information with you to determine your triggers.Conditions that cause seizuresSeizures can happen for many different reasons. These include but aren’t limited to the following:Aneurysms.Brain tumors.Cerebral hypoxia.Cerebrovascular disease.Diabetes.Severe concussion and traumatic brain injury, especially ones with loss of consciousness.Degenerative brain diseases like Alzheimer’s disease or frontotemporal dementia.Eclampsia.Electrolyte problems, especially low sodium (hyponatremia), calcium or magnesium.Epilepsy (seizures that happen frequently without any clear, underlying cause).Genetic conditions.Other conditions that can cause seizures may include:Hormone-related changes.Infections (especially encephalitis, meningitis or sepsis).Inflammation from autoimmune conditions.Mental health issues (known as psychogenic seizures) like conversion disorder.Problems with how your brain developed (congenital brain abnormalities meaning occurring with birth).Strokes.Toxins and poisons (such as carbon monoxide poisoning or heavy metal poisoning).Venomous bites or stings.What are the risk factors for a seizure?Anyone at any age can have a seizure. You may be more at risk if you:Have an underlying medical condition.Have a biological family history of seizures.Are a child (under 18 years).Are over age 50.What are the complications of a seizure?Seizures often involve losing consciousness and passing out. When this happens, there’s a risk of injuries from falling or suddenly stopping what you’re doing at the time (like driving, operating machinery or climbing heights). Convulsions may cause you to smack your arms or legs on hard objects, causing cuts, bruises or broken bones.Status epilepticus happens when a seizure lasts for more than five minutes or you have more than one seizure without enough time between them to recover. Status epilepticus is a life-threatening medical emergency because it can cause brain damage or even death.Seizures and mental healthSeizures can significantly impact your mental health. It’s also common to have symptoms of anxiety and depression with seizures.This may happen because seizures are distracting and can pull you away from the activities you enjoy. You may feel anxious or fearful of having another seizure. You may keep yourself up at night worrying about when the next one might happen. You might avoid going out in public or spending time with loved ones if you’re embarrassed about having a seizure in front of others.Seizures happen outside of your control, so it’s normal to have these feelings. A mental health professional can help you manage how seizures affect your emotional well-being.Diagnosis and TestsHow is a seizure diagnosed?A healthcare provider, usually a neurologist, will diagnose a seizure after a physical exam, neurological exam and testing. During the exams, your provider will learn more about your symptoms and review your medical history and family health history.It often helps to have someone with you during your appointment who witnessed the seizure to explain what they noticed, as you might not remember what happened.What tests diagnose a seizure?Tests may help confirm whether you had a seizure and — if you did — what might have caused it.A key part of diagnosing seizures is finding if there’s a focal point — a specific area in your brain where your seizures start. Locating a focal point can help your provider plan for treatment.Tests to diagnose seizures include:Blood tests.Computed tomography (CT) scan.Electroencephalogram (EEG).Genetic tests.Magnetic resonance imaging (MRI).Positron emission tomography (PET) scan.Spinal tap (lumbar puncture).Providers might also recommend tests if they suspect injuries or complications from a seizure. Your provider will tell you (or someone you choose to make medical decisions for you) what tests they recommend and why.How is a seizure treated?Seizure treatment varies based on the type, severity and cause. Your healthcare provider may recommend the following:Managing any underlying causes or conditions: Your provider will first treat any underlying conditions — like a stroke or low blood sugar. This may prevent future seizures.Taking antiseizure medications: Medications may help prevent seizures or decrease how often they happen.Surgery: Surgery may reduce seizure frequency and severity by addressing the area of your brain where seizures start (focal point).Brain stimulation: A surgeon will implant a device into your brain to deliver a mild electrical current. The current interferes with and tries to stop abnormal electrical activity. There are different types of brain stimulation available, like vagus nerve stimulation.When to see a doctorSeek medical help right away if you have a seizure or if you see someone have a seizure and any of the following happens:The seizure lasts more than five minutes.The person isn't breathing after the seizure stops.A second seizure follows right away.The person has a high fever.The person's body overheats, called heat exhaustion.The person is pregnant.The person has diabetes.The seizure causes an injury.The seizure happens in water.Can a seizure be prevented?Seizures are unpredictable, so it’s not possible to completely prevent them. The best thing you can do is avoid possible causes or triggers, like managing blood glucose levels or protecting yourself from illness and injury.What can I expect if I have a seizure?Fewer than half of people who have a single, unprovoked seizure will have another. If a second seizure happens, healthcare providers may recommend starting antiseizure medications. For provoked seizures, the risk of having another depends on what caused the first seizure. If it’s treatable, your risk of having another seizure is low (unless you have a repeat of the circumstances that caused the first seizure).Medications may prevent seizures or reduce how often they happen. However, it sometimes takes trying multiple medications (or combinations of them) to find one that works best.In some cases, seizures may be more difficult to treat with medications alone. A provider may recommend surgery, following a specific meal plan or other treatment options.If seizures happen often, your provider can help you take precautions to stay safe. You may choose to wear a medical ID bracelet or carry a medical ID card with you so others will know what to do in the event of a seizure.How long does a seizure last?Seizure symptoms usually last for a few seconds to minutes, up to 15 minutes. Symptoms can last longer if you have several seizures, one after the other (this is a medical emergency).
READ MORE